If you’re like most people, you probably think of insulin resistance as something that only affects people with diabetes.
However, insulin resistance syndrome is a very real and serious problem for many people – even those who don’t have gestational diabetes.
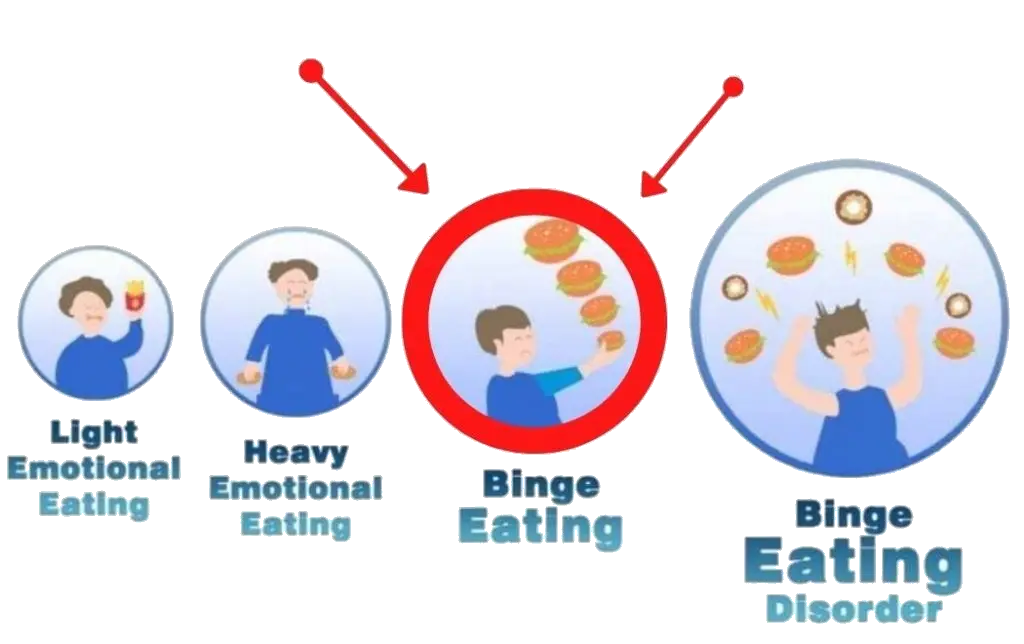
In fact, if you don’t treat insulin resistance via lifestyle modifications and supplements for insulin resistance, it can lead to emotional binge eating and other dangerous health problems.
What is insulin?
Insulin is a hormone produced by the pancreas that helps the body store and use sugar from the food we eat.
When you eat, your body breaks down carbohydrates into glucose (sugar), which then enters your bloodstream.
Insulin signals to your cells to allow glucose to enter, giving them energy and preventing high levels of sugar in the blood. When there’s too much insulin or not enough sensitivity to it, diabetes can develop as well as other health problems related to insulin resistance.
How does insulin resistance affect my health?

Insulin resistance affects your short-term and long-term health. In the short term, it can lead to emotional binge eating and weight gain due to overeating or lack of physical activity.
Long-term, if left unchecked, it can raise blood pressure, cholesterol levels, increase risk for heart disease, stroke, and even cancer.
What is prediabetes?
Prediabetes is a condition where the body’s blood sugar (glucose) levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes.
Prediabetes can lead to type 2 diabetes if it is left untreated. People with prediabetes have an increased risk of heart attack, stroke and other complications due to their increased glucose levels.
Glucose is the main form of energy for the body, and it is regulated by insulin, a hormone produced by the pancreas.
With prediabetes, either the body does not produce enough insulin or cells in the body become resistant to insulin, making it difficult for cells to absorb glucose from the bloodstream. This leads to higher than normal glucose levels in the blood.
Prediabetes can be caused by lifestyle factors such as poor diet, lack of physical activity and obesity. It is important for people who are at risk for prediabetes, or those who have been diagnosed with prediabetes, to make lifestyle changes in order to reduce their risk of developing type 2 diabetes.
These include eating a balanced diet that is low in fat and sugar while also increasing physical activity level; losing weight if necessary; quitting smoking; and controlling cholesterol and blood pressure levels.
The diagnosis of prediabetes is based on two common tests: fasting blood glucose test and oral glucose tolerance test (OGTT).
The fasting blood glucose test measures your blood sugar after you’ve been fasting for 8 hours or more and finds out whether you have abnormally high levels of glucose after not having food or drink for several hours.
The OGTT measures the amount of sugar present in your blood after consuming a sugary drink or food item over a two-hour period; this helps determine how well your body manages its own sugar levels.
If you are diagnosed with prediabetes, there are many steps you can take to prevent or delay progression into type 2 diabetes such as:
- following a healthy lifestyle (eating healthy foods, exercising regularly)
- monitoring your weight regularly
- taking medications such as metformin if prescribed by your doctor
- attending regular checkups with your healthcare provider since early detection of problems related to elevated glucose levels can help prevent further health problems from developing down the road.
What happens if you insulin resistant?
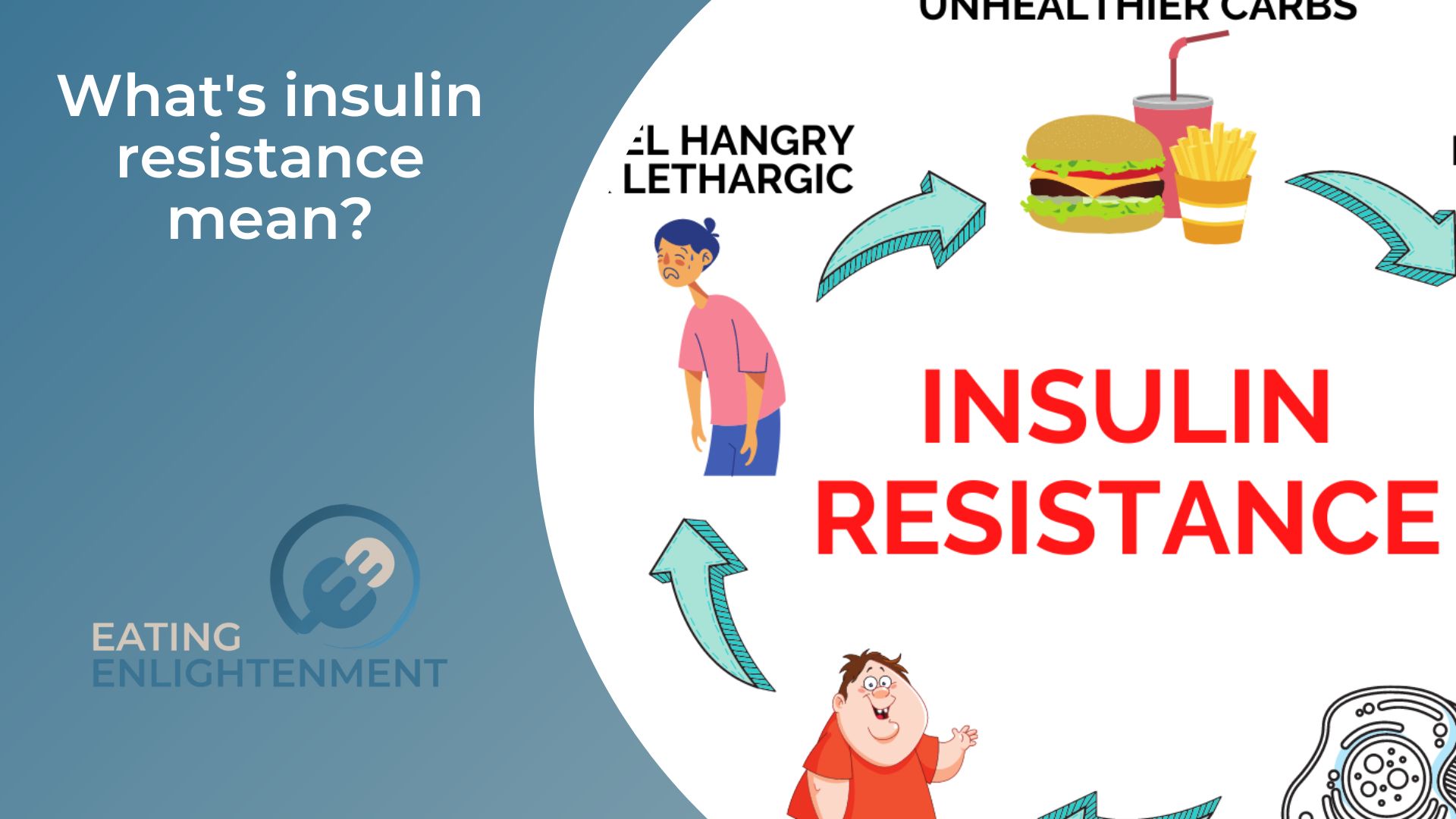
If you develop insulin resistance, your body cannot absorb blood glucose from the food you eat effectively.
This means that glucose will remain in your bloodstream instead of being absorbed by cells and used for energy. Over time, this can lead to a build-up of glucose in the blood and eventually cause type 2 diabetes.
Insulin resistance increases your risk for other complications as well, such as heart disease, stroke, kidney failure and vision loss.
Elevated levels of glucose in the bloodstream can damage blood vessels over time, which can in turn increase cholesterol levels and contribute to cardiovascular disease.
In addition, insulin resistance has been linked to polycystic ovary syndrome (PCOS), non-alcoholic fatty liver disease (NAFLD) and metabolic syndrome – a group of conditions associated with an increased risk of developing type 2 diabetes and heart disease.
Managing your insulin resistance is essential to prevent or delay progression into type 2 diabetes.
Lifestyle modifications like maintaining a healthy weight through proper diet control and regular physical activity help improve insulin sensitivity, allowing glucose to move more easily out of the bloodstream and into cells where it can be used for energy. Eating low glycemic index foods helps regulate blood sugar levels and keeps them within normal ranges.
Medications such as metformin or rosiglitazone (Avandia) may also help control glucose levels if lifestyle modifications alone are not enough to do so.
Additionally, closely monitoring blood glucose levels is important for people with either condition as it helps catch any potential problems before they become serious issues. Regular checkups with doctors are necessary to ensure proper diagnosis and treatment of any issues that may arise from having an elevated level of glucose in the bloodstream.
How do doctors diagnose insulin resistance and prediabetes?
Doctors diagnose insulin resistance and prediabetes through a combination of physical exams, medical history, and blood test options. The most commonly used tests include fasting blood glucose levels, oral glucose tolerance tests (OGTTs), and hemoglobin A1c (HbA1c) levels.
Fasting blood glucose tests measure the amount of sugar in the blood after not having had food or drink for 8 hours or more. If the results are higher than normal, it could indicate insulin resistance, or prediabetes.
The OGTT is similar to the fasting glucose test but measures how well your body manages its own sugar levels after consuming a sugary item over two hours.
During this time, your doctor will also be monitoring your blood sugar levels at regular intervals. If they’re higher than normal at any point, it could mean you have insulin resistance or prediabetes.
The HbA1c test is another option for diagnosing insulin resistance and prediabetes. This test measures the average amount of sugar in your blood over the past three months by analyzing red blood cells.
If these results are higher than usual, it could mean you have elevated glucose levels that signify prediabetes or diabetes.
Your doctor may also perform a physical exam to check for signs of insulin resistance such as:
- weight gain
- dark patches on the skin (acanthosis nigricans)
- high cholesterol levels
- high blood pressure and other conditions associated with metabolic syndromes such as polycystic ovary syndrome (PCOS).
In addition to these tests and exams, doctors may also ask questions about your family history since genetics can play a role in developing insulin resistance or prediabetes.
It’s important to answer these questions honestly so that your doctor can put together an accurate picture of your health and make appropriate recommendations on how to diagnose and treat any issues that might arise from insulin resistance or prediabetes.
Tell me the difference between insulin resistance and prediabetes?
The main difference between insulin resistance and prediabetes is that insulin resistance is a condition in which the body does not respond properly to insulin, while prediabetes occurs when the body’s blood sugar levels are higher than normal but not yet high enough for a type 2 diabetes diagnosis.
Insulin resistance can lead to prediabetes if left untreated. Symptoms of both conditions include fatigue, weight gain, dark patches on your skin (acanthosis nigricans), increased thirst, increased urination and difficulty concentrating.
Prediabetes can also be diagnosed through tests such as fasting glucose or oral glucose tolerance test (OGTT) while insulin resistance may require doctors to perform additional tests such as hemoglobin A1c (HbA1c).
How can I prevent or reverse insulin resistance and prediabetes?
The best way to prevent or reverse insulin resistance and prediabetes is to make healthy lifestyle changes.
- This includes eating a balanced diet, exercising regularly, and maintaining a healthy weight.
- Eating a diet that is low in refined carbohydrates, saturated fats, and added sugars is important for reducing insulin resistance.
- Incorporating plenty of whole grains, fresh fruits and vegetables, lean proteins, and healthy fats into your diet can help keep your blood sugar levels in check and reduce your risk of developing diabetes or its complications.
- Regular physical activity is also essential for managing insulin resistance and prediabetes. Aim to get at least 30 minutes of moderate intensity exercise on most days of the week.
This can help improve your body’s sensitivity to insulin as well as boost your metabolism so you can better manage your blood sugar levels.
Additionally, exercise helps to promote weight loss which can further reduce insulin resistance.
Lastly, it is important to maintain a healthy weight as obesity is one of the main risk factors for developing insulin resistance and prediabetes.
- Eating regular meals with balanced nutrient profiles and limiting refined carbohydrates can help you reach a healthier weight while also improving your overall health.
- If you are already diagnosed with insulin resistance or prediabetes, it is important to talk to your doctor about medications that may be able to help control glucose levels such as metformin or rosiglitazone (Avandia).
- Additionally, following a structured meal plan that focuses on portion control and eating low glycemic index foods can be beneficial for keeping blood sugar levels within normal ranges.
- It is also important to monitor blood glucose levels closely if you have been diagnosed with either condition as this can help detect any potential problems before they become serious issues.
Regular checkups with doctors are necessary in order to ensure proper diagnosis and treatment of any issues that may arise from having an elevated level of glucose in the bloodstream.
How Insulin Resistance Progresses to Type 2 Diabetes?

Insulin resistance is a condition in which the body does not respond properly to insulin, causing elevated levels of glucose to remain in the bloodstream. Over time, this can lead to type 2 diabetes if left untreated.
When insulin resistance occurs, the body does not use glucose effectively, which causes it to build up in the bloodstream.
This results in higher than normal levels of glucose, or hyperglycemia. As the body continues to be exposed to high levels of glucose over an extended period of time, it will eventually become desensitized and less responsive to insulin prompting further increases in glucose concentrations.
As glucose levels increase further and remain consistently elevated, beta cells in the pancreas become overwhelmed by the demand for insulin production and eventually start to fail.
This leads to even higher levels of glucose as insulin’s ability to regulate blood sugar is weakened.
As beta cells continue to be damaged by prolonged exposure to high glucose concentrations, they are unable to sufficiently produce enough insulin for the body’s needs leading ultimately to type 2 diabetes.
Insulin resistance may also cause other complications such as increased risk for heart disease, stroke, kidney failure and vision loss due its effects on blood pressure, cholesterol and other biomarkers associated with cardiovascular disease.
In addition, people with insulin resistance are more likely to develop metabolic syndrome (a combination of conditions that raise heart disease risk), polycystic ovary syndrome (PCOS) and non-alcoholic fatty liver disease (NAFLD).
Proper management of diabetes through lifestyle modification along with diet control and regular monitoring are key ways that individuals can prevent or delay progression from insulin resistance into type 2 diabetes.
Conclusion
In conclusion, insulin resistance is a serious condition that can lead to type 2 diabetes if not managed properly.
Making healthy lifestyle changes such as eating a balanced diet low in refined carbohydrates and saturated fats while increasing physical activity level can help improve weight management which is essential for reducing the risk of developing complications associated with this condition.
Additionally, talking with your doctor about possible medications or treatments may be beneficial if lifestyle modifications alone are not enough to reduce glucose levels in the bloodstream.
Regular checkups with doctors should also be done to ensure proper diagnosis and treatment of any issues that may arise from having an elevated level of glucose in the bloodstream.
With these steps, individuals will have better control over their health and potentially prevent progression into type 2 diabetes.