Insulin resistance is a condition in which your body’s cells don’t respond properly to insulin, leading to high blood sugar levels. It can be caused by obesity, physical inactivity, genetics, and other factors.
Fortunately, there are several tests available to check for insulin resistance and determine how severe it may be.
Knowing if you have this condition can help you make lifestyle changes that could improve your health, including supplements for insulin resistance, and reduce the risk of developing diabetes or other chronic diseases.
In this blog post we will discuss the different methods used to test for insulin resistance so that you can choose the best option for yourself.
What is insulin resistance?
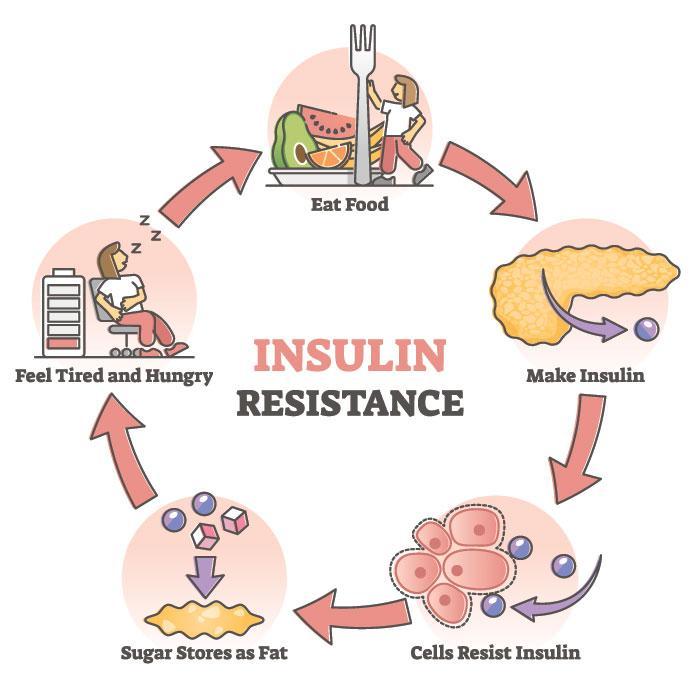
Insulin resistance is a condition in which the body’s cells do not respond properly to insulin, leading to high blood sugar levels.
It can be caused by obesity, physical inactivity, genetics, and other factors. Insulin resistance can increase the risk of developing diabetes and heart disease if left untreated.
Treatment of insulin resistance involves lifestyle modifications such as maintaining a healthy diet and regular exercise.
Some medications may be needed to help manage and reduce the symptoms of this condition. Testing for insulin resistance is important for determining how severe it may be and helping people make informed decisions about their health care needs.
What causes insulin resistance?
People develop insulin resistance due to a number of factors, including obesity, physical inactivity, genetics, and certain medications.
- Obesity is thought to be the most common cause of insulin resistance; when people are overweight or obese, their cells become less sensitive to insulin. This means that more insulin is needed for the cells to absorb glucose from the blood.
- Physical inactivity can also lead to insulin resistance because lack of exercise leads to a decrease in muscle mass and an increase in fat tissue. Fat tissue does not respond well to insulin and can cause cells to become resistant.
- Genetics can play a role as well, as certain genes may make individuals more prone to developing insulin resistance. Finally, certain medications can interfere with how the body processes glucose and make it harder for cells to respond properly to insulin.
Other lifestyle factors
- Stress hormones decrease the body’s ability to use insulin effectively, while inadequate sleep has been linked with changes in hormones that affect how the body responds to glucose levels.
- Eating an unhealthy diet high in processed foods and sugar can also contribute; these foods have been shown to increase inflammation throughout the body which makes it harder for cells to respond appropriately to glucose levels.
How do I know if I’m insulin resistant?

The best way to know if you are insulin resistant is to see your doctor and get tested.
You can do a fasting glucose test or an oral glucose tolerance test (OGTT) that measures how quickly the body breaks down and absorbs sugars over a two-hour period.
Fasting insulin levels, postprandial glucose levels (after eating), HOMA-IR, and euglycemic clamp studies can also be used to measure and diagnose insulin resistance.
If any of these tests show elevated results then you may have insulin resistance or type 2 diabetes. It’s important to get checked out by a professional for an accurate diagnosis.
The CDC says, “How do you find out if you’re insulin resistant? No one test will tell you, but if you have high blood sugar levels, high triglycerides (a kind of blood fat), high LDL (“bad”) cholesterol, and low HDL (“good”) cholesterol, your health care provider may determine you have insulin resistance.”
How do doctors diagnose insulin resistance and prediabetes?
Doctors typically diagnose insulin resistance and prediabetes through a combination of tests. The most common test used is a fasting blood sugar test, which measures the amount of glucose in the blood after an overnight fast.
Another common test is the A1C test, which looks at average levels of glucose over the last two to three months. Other tests that can be used to diagnose insulin resistance include an oral glucose tolerance test and a random blood sugar test.
In addition to these tests, doctors may also use additional tests to assess insulin sensitivity and determine how severe a patient’s insulin resistance is.
These include a homeostasis model assessment (HOMA) and an euglycemic clamp. The HOMA test measures how well insulin is regulating glucose in the body, while the euglycemic clamp looks at how quickly cells respond to changes in glucose levels.
If any of these tests come back indicating prediabetes or diabetes, then doctors may order additional tests to check for any underlying conditions such as hormonal imbalances or organ-related complications that could be causing elevated levels of glucose in the blood.
These could include tests like a C peptide level, thyroid function panel, or kidney function panel.
The diagnosis of insulin resistance and prediabetes should always be followed up with lifestyle modifications such as dietary changes and increased physical activity in order to reduce risk factors for developing diabetes and other chronic diseases associated with it.
Additionally, your doctor may prescribe medications if necessary to help manage the condition.
How can insulin resistance cause all these widespread problems?
Insulin resistance can cause a variety of health problems because it affects the body’s ability to regulate glucose levels.
When cells become resistant to insulin, they cannot absorb glucose from the blood as effectively and this leads to elevated glucose levels in the body. Over time, high levels of glucose wreak havoc on various organs; it damages small blood vessels which can slow down circulation and lead to an increased risk for stroke and heart attacks.
Too much sugar in the bloodstream also causes inflammation throughout the body, which can lead to other chronic diseases such as obesity, type 2 diabetes, depression, dementia and cancer.
Also insulin resistance is linked with hormonal imbalances like PCOS which can cause fertility issues in women or contribute to obesity or diabetes later in life.
And most importantly long-term elevated glucose levels also increase oxidative stress within cells which leads to damage from free radicals and accelerates aging throughout the entire body.
How can I prevent or reverse insulin resistance and prediabetes?
Preventing or reversing insulin resistance and prediabetes begins with lifestyle changes.
- Eating a healthy, balanced diet low in processed foods and added sugars is the foundation of this effort.
- Incorporating plenty of fruits and vegetables, as well as whole grains, legumes, nuts, seeds, lean proteins and healthy fats can help reduce inflammation throughout the body while providing adequate fuel for cells.
- Eating regularly scheduled meals throughout the day with appropriate portion sizes is also important for managing glucose levels.
- Regular physical activity is essential for reducing insulin resistance and prediabetes risk. Regular aerobic exercise like walking or jogging has been shown to improve insulin sensitivity.
- Strength training is also important for building muscle mass which increases cell sensitivity to glucose levels. Aim for at least 30 minutes of moderate-to-high intensity exercise per day spread out over several days each week.
In addition to lifestyle changes, doctors may also recommend medications such as metformin or thiazolidinediones (TZD) to help reduce insulin resistance.
These medications are designed to help cells respond more efficiently to glucose levels in the blood while decreasing inflammation throughout the body.
However, they should not be used as a substitute for lifestyle changes; instead these medications should be used in combination with diet and exercise modifications for maximum effect.
It’s also important to manage stress levels as best as possible since chronic stress can worsen insulin resistance due to increased cortisol levels associated with it.
Stress reduction techniques like deep breathing exercises and yoga are good ways of calming the mind and body while improving overall wellbeing.
Meditation can also be beneficial by helping individuals become more aware of their thoughts and feelings which allows them to develop better coping mechanisms when faced with stressful situations.
Why a fasting glucose test isn’t enough?
A fasting glucose test is not enough to accurately detect insulin resistance and/or prediabetes because it only measures your glucose levels after a period of fasting.
Insulin resistance can present with normal or even low fasting glucose levels, so the only way to truly measure insulin sensitivity is by taking an oral glucose tolerance test (OGTT) which involves drinking a sugary liquid and then monitoring blood sugar levels over a two-hour period.
This gives doctors more accurate information about how quickly the body breaks down and absorbs sugar, indicating whether cells are resisting insulin or not.
Furthermore, if someone’s results reveal impaired fasting glucose but normal postprandial (after eating) readings on OGTT results then they likely don’t have diabetes but may be at risk for developing it in the future.
Therefore, a fasting glucose test alone is insufficient to accurately assess insulin resistance and/or prediabetes; doctors must also take into account OGTT results when diagnosing these conditions.
Types of Insulin Resistance Tests
There are several tests that can be used to measure and diagnose insulin resistance, as well as blood glucose levels.
The most common test is the fasting glucose test, which measures your blood sugar levels after a period of fasting. This test is typically used in combination with an oral glucose tolerance test (OGTT) for better accuracy – the OGTT measures how quickly the body breaks down and absorbs sugars over a two-hour period.
Other tests that may be used include fasting insulin levels, postprandial glucose levels (after eating), HOMA-IR, and euglycemic clamp studies.
The fasting plasma glucose test is usually the first step in diagnosing insulin resistance. This simple finger prick test measures your blood glucose level after an 8-10 hour fast.
If your results are higher than normal, it could indicate pre-diabetes or diabetes, but this should not be taken as a definitive diagnosis – doctors will usually do an OGTT to confirm their suspicions.
Insulin levels may also be tested during the fasting glucose test; if they’re elevated then it could mean you have insulin resistance or type 2 diabetes.
The oral glucose tolerance test (OGTT) is another commonly used diagnostic tool for measuring insulin sensitivity and pre-diabetes/diabetes risk factors.
This involves drinking a sugary solution and then testing your blood sugar 25 minutes later, then again after 1 hour and 2 hours later.
When compared with your initial fasting readings, this gives doctors a much clearer picture of how efficiently cells are responding to sugar levels in the bloodstream – if people have impaired postprandial (after eating) results on OGTT tests then they likely don’t have diabetes but may still be at risk of developing it in the future.
The HOMA-IR test measures your homeostatic model assessment index of insulin resistance by comparing your fasting insulin and glucose levels to calculate an estimated measure of insulin sensitivity/resistance.
It’s often used as a screening tool when other methods such as OGTTs cannot be conducted due to time constraints or other reasons.
Finally, euglycemic clamp studies involve infusing sugar into the bloodstream while simultaneously measuring changes in circulating hormones like cortisol and catecholamines that can affect blood sugar balance; these readings give doctors more detailed insights into how well cells are responding to different concentrations of sugar in the blood.
Endocrine issues caused by Insulin Resistance
Problem: Insulin resistance can lead to a variety of endocrine issues, such as weight gain, fatigue, and increased risk for type 2 diabetes.
Agitate: If left untreated, insulin resistance can cause serious health problems like high blood pressure and heart disease. It’s important to catch this condition early on in order to prevent long-term damage.
Solution: The best way to diagnose insulin resistance is through a combination of tests including fasting glucose test and oral glucose tolerance test (OGTT).
These tests measure your body’s response to sugar levels in the bloodstream and give doctors more accurate information about how quickly cells are breaking down sugars.
Other tests that may be used include HOMA-IR or euglycemic clamp studies which provide even more detailed insights into how well cells are responding to different concentrations of sugar in the blood.
By getting tested regularly you can stay ahead of any potential endocrine issues caused by insulin resistance before they become serious health problems.
Clinical trials
Clinical trials are an essential part of researching and developing effective treatments for insulin resistance.
Through clinical trials, researchers can study the effects of different medications and other treatments on patients with insulin resistance in order to determine which ones are most effective.
Clinical trials provide invaluable evidence about the safety and efficacy of new drugs, as well as data that can be used to inform clinical practices.
One form of clinical trial commonly used in the treatment of insulin resistance is a randomized control trial (RCT).
In an RCT, participants are randomly assigned to receive either the experimental intervention or a control intervention such as a placebo.
This type of study allows researchers to compare outcomes across different groups, helping them identify any potential benefits or risks associated with the treatment being tested.
Clinical trials have also been used to evaluate lifestyle interventions for improving insulin sensitivity.
For example, a 2020 study found that a low-fat vegan diet was more effective than a low-calorie diet for improving insulin sensitivity and reducing body mass index (BMI) among people with type 2 diabetes.
Lifestyle modifications such as physical activity and dietary changes may also help reduce risk factors associated with insulin resistance, such as obesity and high blood pressure.
In addition to evaluating drug therapies and lifestyle interventions, clinical trials can provide important insights into the pathophysiology of insulin resistance.
By monitoring biomarkers before, during, and after treatment, researchers can gain valuable insight into how different treatments affect cellular pathways involved in glucose metabolism.
Such information can aid in designing successful strategies for treating and preventing this condition from progressing further.
Overall, clinical trials play an essential role in helping clinicians understand how best to treat and manage individuals with insulin resistance.
Through rigorous testing of various therapies and interventions, researchers can identify those that offer the greatest benefits while minimizing any potential risks associated with them.
With these findings in hand, healthcare providers can confidently provide their patients with evidence-based treatment plans tailored to their individual needs.
Conclusion
Insulin resistance is a serious condition that can have devastating effects on one’s health if left untreated. Fortunately, there are many ways to diagnose and treat insulin resistance before it leads to more severe medical issues.
Through the use of tests such as OGTTs and HOMA-IR studies, doctors can catch this condition early on in order to prevent long-term damage.
Clinical trials also play an important role in helping clinicians understand how best to manage individuals with insulin resistance by evaluating different treatments for effectiveness and safety.
With these findings, healthcare providers can confidently provide their patients with evidence-based treatment plans tailored specifically for their individual needs.
Ultimately, understanding the causes of insulin resistance and taking steps towards prevention or management will help ensure better overall health outcomes for those affected by this condition.