Ok, here’s a really common but confusing eating situation, see if you can relate.
- Katherine is a 40 year-old woman whose weight is pretty normal for her age. She’s trying, like many of her friends, to lose weight by eating clean foods, thinking about calories and trying her best to exercise.
- A few times per year she tries a new diet, or goes back to Weight Watchers.
- In the background of Kat’s mind is a constant chatter of calories, good and bad foods. It’s like she has both an angel and devil on her shoulder and neither one of them will shut the f**k up!
- A couple times a month Katherine goes on a ravenous binge. She always binges on the foods that she’s not supposed to eat.
- Horrible pangs of guilt and shame follow quick. Katherine starts to wonder if she has an eating disorder so she researches binge eating disorder criteria.
- Katherine finds out that Binge Eating Disorder means you distressfully binge “at least 1 day a week for 3 months”.
- But Katherine only binges around 2-3x per month so she doesn’t meet the criteria for binge eating disorder or other common eating disorders.
- Katherine feels like she has a problem with food, but she doesn’t have a label or any sort of language to make sense of her problem.

Can you relate?
You don’t have Binge Eating Disorder, but you have a problem with food.
If you can relate, this post is going to give you clinical language to diagnose your problem. It turns out there is a catch-all clinical term with the acronym OSFED. I’ll explain what that means down below.
And I know official clinical diagnoses can be disturbing some people. I will talk about being negatively labeled by others and stigma later on in this post. However, for many people who feel confused about food, the OSFED type of language can be incredibly helpful even if you don’t have an official diagnosis.
I hope you keep that in mind as you read this article.
Let’s dive in. This post will first cover Binge Eating and give a general overview of eating disorder statistics. Then I’ll dive more into the clinical language. Specific topics include:
- Binge Eating & Eating Disorder Statistics
- What Are The Most Common Eating Disorders?
- About OSFED Diagnosis, Stigma, and Labeling
- OSFED Symptoms
- Prevalence of ‘Disordered Eating’
- Eating Disorder Treatment Outcomes
Below is a video where I discuss some of the facts about eating disorders, and offer my opinion on various treatment issues for both men and women:
Binge Eating & Eating Disorder Statistics
If you feel bad about your eating struggles, hopefully the following information can put things into perspective.
(You’ll still probably feel crappy afterwards, but if you can wrap your mind around how common eating struggles are, you’ll feel a bit better)
For starters, 30 million people of all ages, genders and socioeconomic status suffer from official, clinically diagnosable eating disorders in the United States.
Overall there are more women than men who suffer from eating disorders.At the eating disorder outpatient clinic where I work, we do see about 1:3 men to women ratio.
While women are more likely than men to get an eating disorder, the prevalence of all types of eating disorders, including anorexia nervosa and bulimia nervosa, are sadly on the rise for men as well.
Now let’s put aside the eating disorder statistics for gender. Let’s just focus on the big picture.
Overall, approximately 10% of the U.S. population struggles with clinical eating disorders (the eating disorder categories that Katherine did not qualify as being in).
Now out of these 30 million people (approximately 10% of the population), there is a range of eating disorders. The following is one of the most frequently asked questions I see:
Generally Speaking, What Are The Most Common Eating Disorders?
The most commonly known eating disorders to the general public are:
- Binge Eating Disorder
- Bulimia Nervosa
- Anorexia Nervosa (anorexia has the highest mortality rate)
(Please note how I use the term ‘commonly known’ here, because as you’ll find out, there is a type of eating disorder that is more common, but not as well known).
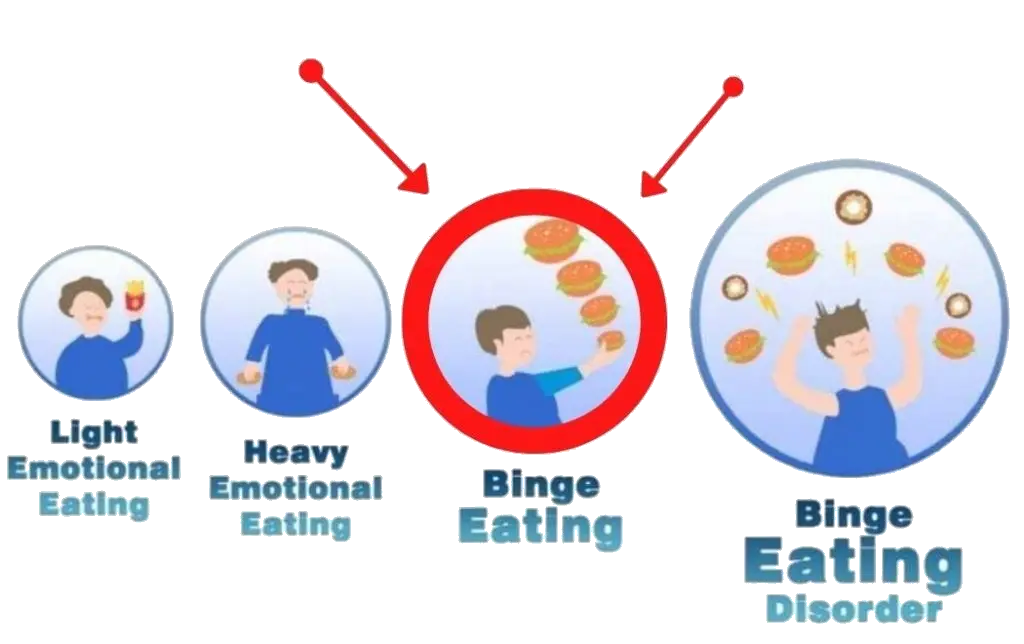
Binge Eating Disorder (which is the focus of this blog, along with emotional eating and disordered eating which are less severe forms of binge eating disorder) is three times more prevalent than bulimia and anorexia combined.
Binge Eating Disorder also is more common than breast cancer, HIV and schizophrenia.
Although on some level, it doesn’t matter which eating disorder is most common. All of these have drastic consequences for mental health! Additionally, all eating disorders have similar treatment approaches as well, which I’ll talk about in the last section.
(If you’re curious where I got that information, here’s my source: Hudson JI, Hiripi E, Pope HG Jr, and Kessler RC. (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3):348-58. doi:10.1016/j.biopsych.2006.03.040.)
Here’s the point:
Binge Eating Disorder is incredibly common!
Binge Eating is so common. That’s the point.
In fact, it’s so common (and even more common than breast cancer), that I’m going to ask you to see Binge Eating Disorder like you would breast cancer, in terms of individual responsibility (note I’m not saying here that Binge Eating Disorder is the same as breast cancer in terms of mortality rates,).
Here’s what I mean:
My friend’s mom got breast cancer a few years ago, and she lived, thank god. But nobody at any point in time ever blamed her for developing cancer.
It wasn’t her fault for developing cancer.
All of us know that breast cancer is something that many people suffer from, and that getting it had nothing to do with individual responsibility.
So as we continue to look at eating disorder statistics, I’d like you to have a compassionate mindset. There are sooo many people struggling and it’s not their fault!
(I know, some of you will say that Binge Eating might seem like it’s the person’s fault, unlike cancer, but that’s not the right way of viewing eating disorders.)
If you don’t have time to read the article, no problem. I’ll give you the short story here:
50% of Binge Eating Disorder is genetic, and I’ll cover some other reasons which exonerate individuals down below.
And please note that while the individual is not to blame, part of life is accepting responsibility for problems that you didn’t cause yourself. So while I’m not blaming the individual, I’m also not saying the individual person in question can just do nothing either.
This conversation on the origins of Eating Disorders ties nicely into another frequently asked question:
How To Get A Eating Disorder?

That’s right, many eating disorders are significantly genetic. Incredible huh?
When 50% of the disorder is genetic, it’s hard to blame someone’s lack of responsibility.
When you hear other statistics about eating disorders in the future, just keep in mind that it’s NOT an issue of personal responsibility.
Furthermore, as your education about eating disorders increases, you will see another clear pattern:
Dieting and weight loss at a young age also contribute to (or even directly cause) eating disorder statistics.
(And when you’re age 13 and ‘decide’ to diet, are you really responsible for your decisions?)
Essentially, statistics show that people with clinical eating disorders statistics are genetically prone to eating disorders and that they also dieted at a young age.
The National Institute of Mental Health reports “There is a commonly held misconception that eating disorders are a lifestyle choice”.
That’s the assumption that I feel many people hold about eating disorders, including anorexia nervosa and bulimia nervosa, and about mental health in general.
We assume that bulimia nervosa is a choice. We assume that anorexia nervosa is a bad habit.
The National Institute of Mental Health notes for bulimia nervosa and anorexia nervosa, both are caused by “a complex interaction of genetic, biological, behavioral, psychological, and social factors.”
There are various other factors behind eating disorder statistics too.
- a family member who has an eating disorder
- A highly competitive environment where external success (like having good grades) is promoted
- A person with a naturally bigger body will face weight stigma and fat discrimination in our society. It’s just the tough truth. This person will get the implicit and explicit message that fat is bad, and they will try to lose weight. Sadly, this trying to lose weight is what often causes eating disorders in the first place!
Overall, there’s no person to blame here, so hopefully you can see a bit more now why blaming yourself for your eating struggles is too shortsighted. You may still feel crappy, but knowing there are other factors at play here that you didn’t have much control over can help pave the road to self-forgiveness.
Here are some other eating disorder statistics:
- Around 3% of adults in the United States suffer from Binge Eating Disorder at some point in their lives.
- Up to 30-40% of people searching for weight loss treatments can meet the clinical criteria for Binge Eating Disorder
- The National Comorbidity Survey show that 50% of Binge Eating Disorder people have depression or anxiety.
- 0.9% of women will struggle with anorexia nervosa in their lifetime
- 1.5% of women will struggle with bulimia nervosa in their lifetime
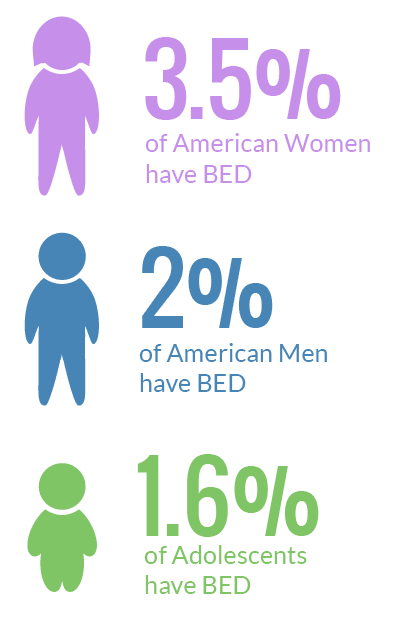
- 3.5% of women will struggle with binge eating disorder
- 0.3% of men will struggle with anorexia nervosa
- 0.5% of men will struggle with bulimia nervosa
- 2% of men will struggle with binge eating disorder
- Anorexia has the highest fatality rate of any mental illness.
Please take note of the National Comorbidity Survey data. The Comorbidity Survey sounds like ‘morbid’, but these data simply show that many people can have two disorders at once. For example, girls with anorexia might also have depression.
In fact, the rate of any mental disorder type increases along with eating disorders. These comorbidity surveys just go to show you how intertwined eating is with our mental health.
Ok, I feel like I’ve beaten eating disorder statistics to a pulp right now.
Are you ready to move on? Let’s switch gears and focus on the other form of eating struggles with which Katherine identifies.
To refresh your memory briefly, Kat struggles with eating, but she isn’t clinically diagnosable for binge eating, anorexia or bulimia. She feels confused about her problems, but has no language.
What Eating Disorder Is ACTUALLY MOST Common?
Fortunately, there is another newer eating disorder diagnosis that most people are unaware of known as Other Specified Feeding and Eating Disorder (OSFED). I consider this term to be synonymous with ‘disordered eating’.
What does OSFED mean?
OSFED is a clinical definition that acts as a net to catch people who fall through the traditional criteria needed for the most commonly known eating disorders of anorexia nervosa, bulimia nervosa, and binge eating disorder.
OSFED is where you have one or a combination of the following two symptoms: distressing eating habits and obsessive weight and body image thoughts.
Estimates say 30-50% of people with eating disorders actually get OSFED.
However, eating disorders statistics usually only mention binge eating, anorexia nervosa, or bulimia nervosa. That’s why earlier I mentioned ‘commonly known‘.
But the reality is that OSFED is by far the most common eating disorder diagnosis for both males and females, across ages.
About OSFED Diagnosis, Stigma, and Labeling

First of all, Katherine in this blog article would fit the criteria for disordered eating or OSFED.
However, Katherine is not a real person. She’s an avatar based off of two past clients of mine, both of whom struggled with disorders, eating, and food but didn’t meet criteria for Binge Eating Disorder. Sorry to disappoint!
One of my past clients felt relieved that the OSFED label existed. She felt a sense of relief knowing that there was a clinical definition that gave her disorders, eating struggles and experiences a form of validation and recognition.
Knowing that this diagnosis was the most common eating disorder according to eating disorder statistics allowed her to more easily tap into a sense of self-compassion instead of self-criticism.
She felt validated. But my other client who struggled with emotional eating didn’t like this label.
This client felt that the OSFED label created a stigma, and made her more susceptible to feeling like a failure. Previously she had felt sort of normal with her emotional eating struggles. But after hearing about OSFED she felt excluded and different.
Hearing her concerns, I immediately let her know that she didn’t have to accept this label for herself. I said that this label was simply a way to give recognition to a common problem. The intention behind the label was not to exclude her, but to include her.
She didn’t mind the OSFED label after our conversation, and it wasn’t a big deal after that.
So I just want to share that if the label helps you, great. But if the label doesn’t help you, forget about it. The label OSFED or Binge Eating Disorder is not necessary to stop emotional and binge eating. It’s just a word.
Let’s dive into the detailed classification and symptoms of OSFED.
OSFED ‘Disordered Eating’ Classification:
There are 5 classifications within OSFED (Other Specified Feeding and Eating Disorder) that are clinically recognized.
- Atypical Anorexia Nervosa (AN): All of the criteria for AN are met, except that despite significant weight loss, the individual’s weight is within or above the normal range.
- Bulimia Nervosa (BN) of low frequency and/or limited duration: All of the criteria for a diagnosis of BN are met, except that the binge eating and inappropriate compensatory behaviors occur, on average, less than once a week and/or for less than 3 months.
- Binge Eating Disorder (BED) of low frequency and/or limited duration: All of the criteria for BED are met, except that the binge eating occurs, on average, less than once a week and/or for less than 3 months. (See the difference here between OSFED and Binge Eating Disorder?)
- Purging Disorder: Recurrent purging behavior to influence weight or shape (e.g., self-induced vomiting, misuse of laxatives, diuretics, or other medications) in the absence of binge eating.
- Night Eating Syndrome: Recurrent episodes of night eating, as manifested by eating after awakening from sleep or by excessive food consumption after the evening meal. There is awareness and recall of the eating. The night eating is not better explained by external influences such as changes in the individual’s sleep-wake cycle or by local social norms. The night eating causes significant distress and/or impairment in functioning.
OSFED Symptoms
OSFED includes a range of emotional, mental, physical and behavioral symptoms.
Please note that for each of the symptoms, it’s in the range of abnormal even if it sounds normal. For example, one of the items down below is ‘skipping a meal’.
While every person from time to time skips a meal, people with an OSFED diagnosis and who struggle with food will routinely skip meals. Just keep that in mind as you read through the symptoms down below, that each symptom can be taken to an extreme level.
OSFED Behavioral Symptoms:
- Extreme exercise as compensation
- Wearing baggy clothes all the time to hide body
- Purging and vomiting
- Binge eating
- Social isolation and avoidance of eating with others
- Inability or denial to feel hunger
- Skipping meals, avoiding certain foods
- Using laxatives, drinking tons of water, or using breath fresheners
OSFED Emotional Symptoms:
- Very self-critical
- Get frustrated at little things that starts off another binge
- Very needy and seeks validation
- Depression
- Anxiety
- Low self-esteem
OSFED Physical Symptoms:
- Yo-yo dieting
- Weight fluctuations
- Dry skin
- Cold often
- Sleeping difficulty
- Muscle weakness
Ok … Whew!
That was a lot of symptoms and technical jargon.
Hopefully you get the point: OSFED is where you struggle with food, but aren’t quite diagnosable with the traditional eating disorder labels.
With that being said, let’s move onto a discussion about some other eating disorder statistics about OSFED.
Prevalence of ‘Disordered Eating’
Please note this section is somewhat controversial, and rational people can agree to disagree.
Here I propose 50% of clinical eating disorders are for OSFED. However, I believe that OSFED actually affects a much, much larger number of people who never get diagnosed.
Now, it’s no secret that for all types of disorders – addiction, personality, mood, etc. – the number of people who have the disorder are significantly more than the number of people who actually receive a clinical diagnosis.
The 2 main reasons for this are simple:
- not everyone has access to medical care
- stigma prevents people from getting care and diagnosis
Some estimates say that only 1/3 or 1/5 of people get diagnosed, who otherwise could have been diagnosed.
Here’s my back of the envelope math calculations:
- If 30 million Americans have an eating disorder, and 50% of those have OSFED, that would mean 15 million people
- 15 million times 3 or 5 (to account for the underdiagnosis estimates I just quoted) equals 45 or 75 million people
So by these estimates, the number of people who actually could qualify for OSFED is between 45-75 million people.
But I think the number of people who have OSFED is more than double this!
Here I’ll provide my rationale and math calculations to end up at a significantly higher number.
My working assumption is that approximately 50% of Americans are actively trying to lose weight each year.
This is based on a study from the Center of Disease Control and Protection which reports that “In 2013–2016, 49.1% of U.S. adults tried to lose weight in the last 12 months.”
That’s approximately 150 million people, each year, trying to lose weight. (Furthermore, 95% of diets don’t work — half of the people who diet regain any lost weight while the other half regains additional weight, so they are heavier than they were before dieting.)
The implication is that 50% Americans are trying to lose weight via dieting and other intentional weight loss methods, but they regain the weight and try again soon thereafter.
This is a significant eating disorder that is not covered by the current OSFED definition.
In my opinion, this situation where someone tries repeatedly to lose weight and then regains the weight should also be considered OSFED.
When you look at America’s food struggles from this perspective, it makes total sense.
We have brain washed ourselves into thinking that intentional weight loss works (but it doesn’t) and we keep on trying no matter what negative mental health outcomes we experience.
We blame ourselves, and we never blame the diet.
And by dieting and weight loss, I’m also using including situations like:
- Fruit and veggies cleanses; where you cut out certain food groups – this is definitely dieting just by another name!
- Casually skipping meals, avoiding food groups on a regular basis, and other compensation methods – even if these behaviors are done without officially being on a diet
- Keto, Paleo, Low Carb, Mediterranean or any of the other diets that have certain foods that you eat and avoid other foods which are bad
Now is it controversial to say that 50% of America should be clinically diagnosed with OSFED?
It’s true, I am biased. Let me know in the comments below.
Treatment Outcomes
One thing that is indisputable is that treatment saves lives. The mortality rates of serious, clinical AND untreated eating disorders, especially anorexia nervosa, can be as high as 20% for young women.
With treatment those mortality rates go down to 2-4%. While the mortality rates are still scarily high, it’s a helluva lot better than no treatment at all.
One of the facts about eating disorders is pretty simple.
The treatment approaches are all very similar, for both men and women.
For example, for every type of eating disorder, all treatment approaches emphasize regular eating, for both women and men no matter what their age or history of eating.
The gold standard treatment for eating disorders is Cognitive Behavioral Therapy (CBT).
Intuitive Eating I feel adds the spiritual and cultural to what CBT misses.
With all of this being said, I hope these facts about eating disorders (and opinions!) can help you understand more about treatment options and perspectives to help you or a loved one heal.